African Americans are dying from the coronavirus at almost 3 times the rate of their white counterparts.
Black and Hispanic Americans were disproportionately more likely to die of COVID-19 during the spring and summer months indicating that the coronavirus’s toll is falling most heavily on underserved and minority communities, according to the Centers for Disease Control and Prevention (CDC).
African Americans are nearly three times more likely to die from COVID-19 compared to white Americans, the @CDCgov estimates. Members of the medical community worry whether one of the most at-risk populations will be unwilling to be vaccinated.https://t.co/wIhOr3X8i5
— Side Effects Public Media (@SideEffectsNews) December 2, 2020
When you consider that African Americans represent 12.5 percent of the population, but account for almost 23 percent of all coronavirus deaths, the COVID-19 pandemic is disproportionately decimating the black working class communities across the country.

Coronavirus has become the third leading cause of death of citizens in the United States in calendar year 2020. The virus has killed more than 300,000 since arriving on U.S. shores, making it a leading cause of death after heart disease and cancer.
In 2018, the 10 leading causes of death for all Americans (heart disease, cancer, unintentional injuries, chronic lower respiratory diseases, stroke, Alzheimer disease, diabetes, influenza and pneumonia, kidney disease, and suicide) remained the same as in 2017. The 10 leading causes accounted for 73.8% of all deaths in the United States in 2018.
The Centers for Disease Control and Prevention (CDC) maintains a provisional death count related to COVID-19. The deaths counted in that data are well below those compiled from the state and county levels because the provisional count is based on death certificates that may take weeks to filter up to the federal agency.
With respect to controlling the pandemic, Martin Luther King Jr. once declared “Whatever affects one directly, affects all indirectly.” This is definitely true for epidemiology and controlling the pandemic. To protect the health of all us, we must insure the health of the most vulnerable among us.
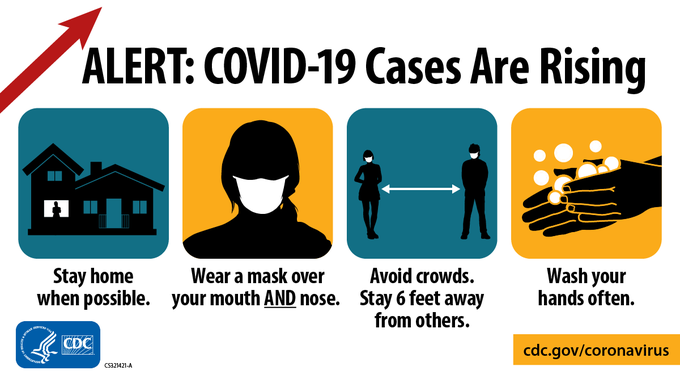
How to control COVID-19 is not a mystery — it requires wearing masks, social physical distancing of 6 feet, frequent washing of hands, widespread contact tracing and COVID testing and widespread vaccination. However, these efforts to combat the pandemic require people to trust the science and those behind the public health measures.
In the nationwide fight against the COVID-19 pandemic, well founded mistrust has developed over decades by African Americans of the government, public health officials and ‘the science’ can and has killed a disproportionate share of working class Blacks and other people of color.
References: