COVID-19 Cases Are Dropping Fast. Four reasons: social distancing, seasonality, seroprevalence, and shots.
COVID-19 is in retreat in America. New daily cases have plunged, and hospitalizations are down almost 50 percent in the past month. The reason for the decline range Americans’ good behavior in the past month combined with (mostly) warming weather across the Northern Hemisphere has slowed the pandemic’s growth; at the same time, partial immunity and vaccines have reduced the number of viable bodies that would allow the coronavirus to thrive.
Fighting disease once meant prioritizing fresh air. How did we forget such a simple lesson? @sarahzhang reports: https://t.co/9gH2oHrH4f
— The Atlantic (@TheAtlantic) February 22, 2021
The current decline of COVID-19 is crystal clear.
There has been a five-week downward trend in cases, according to data collected by the Centers for Disease Control and Prevention. The highest 7-day moving average occurred on January 11, 2021 and was 249,048. The current 7-day average is 77,385 cases, which is a 68.9% decline.
Furthermore, the 24.5% decrease in the 7-day average number of daily cases reported compared with the prior week also provides an encouraging sign of recent progress. Even with these declines, however, the 69,165 cases reported on February 17 remains higher than what was seen during either of the first two peaks in the pandemic.

Daily Trends in COVID-19 Cases
The numbers of new hospital admissions of patients with confirmed COVID-19 have decreased from the national peak of 18,006 admissions on January 5, 2021 to 6,841 admissions on February 16 (a 62% decrease). The average number of daily admissions fell by 21.8% compared to the previous week.
Nationally, the number of COVID-19 deaths continue to fluctuate. There has been over 500,000 total COVID-19 deaths reported with 2,601 new deaths reported as of February 23, 2021. The 7-day average number of new deaths decreased by 9% to 2,708** new deaths per day compared to the previous 7-day period.
Why the decline?
Americans’ good behavior in the past month combined with warming weather across the Northern Hemisphere to slow the pandemic’s growth; at the same time, partial immunity and vaccines have reduced the number of viable bodies that allow the coronavirus to thrive.
According to a piece that ran in the Atlantic.:
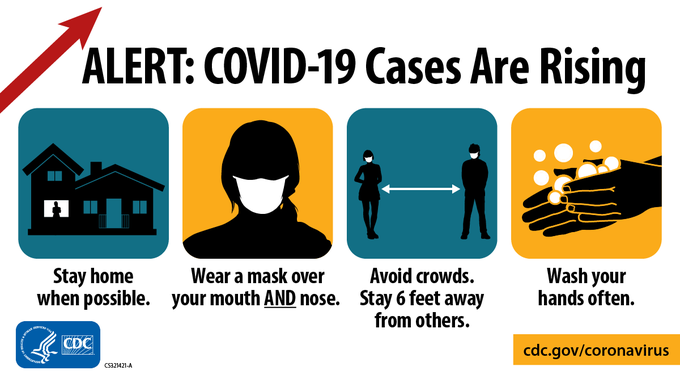
1. Behavior: Americans finally got on board with wearing a mask and social-distancing thing.
Officials pointed to Google mobility data that demonstrated that Americans withdrew into their homes after the winter holidays and hunkered down during the subsequent spike in cases that grew out of holiday season socializing. New hospital admissions for COVID-19 peaked in the second week of January—another sign that social distancing during the coldest month of the year bent the curve.
2. Seasonality: The coronavirus is perhaps seasonal and destined to decline.
Behavior can’t explain everything regarding the decline. Mask wearing, social distancing, and other virus-mitigating habits and behaviors had some impact. But bottomline, COVID-19 is in retreat across North America and Europe. Since January 1, daily cases are down 70 percent in the United Kingdom, 50 percent in Canada, and 30 percent in Portugal. This raises the possibility that SARS-CoV-2, the virus that causes COVID-19, is seasonal.
Many viruses fare best in cold and dry conditions; they’re not well designed to thrive in warmer, sunnier, and more humid outdoor areas, Harvard epidemiologist Michael Mina told New York magazine. Each virus is a bundle of genes and protein encased in a fatty lipid molecule. This fatty shell breaks down more easily in warmer and more humid environmental conditions.
3. Partial immunity: The virus is running out of bodies to infect
The coronavirus needs bodies in order to survive and replicate, and it now has access to fewer welcome hosts. Fifteen to 30 percent of American adults have already been infected with COVID-19, according to CDC estimates.
America’s seroprevalence—that is, the number of people with coronavirus antibodies from a previous infection—is probably concentrated among people who had little opportunity to avoid the disease.
This is partial immunity among the very populations that have been most likely to contract the disease, perhaps narrowing the path forward for the original SARS-CoV-2.
4. Vaccines: Despite naysayers and a few reluctant family members, the shots work.
The vaccines are highly effective at preventing infection. But preventing infection is not all they do. Among those infected, they also reduce symptomatic illness. And among those with symptoms, they reduce long-term hospitalization and death to something like zero.
It’s simple to show why this period of declining hospitalizations should keep going. Assuming the CDC is correct that about 25 percent of adults have COVID-19 antibodies from a previous infection and add to that number the 10 percent of adults who have received vaccine shots since December, that would mean one-third of adults currently have some sort of protection, either from a previous infection or from a vaccine. Thus, sometime this spring, half of American adults should have some kind of coronavirus protection.
"Americans’ good behavior in the past month has tag-teamed with (mostly) warming weather across the Northern Hemisphere to slow the pandemic’s growth," @DKThomp writes: https://t.co/ztuKOAFcDQ
— The Atlantic (@TheAtlantic) February 18, 2021
Although the pandemic is far from over, the U.S. has reached the beginning of the end of COVID-19 as a threat to the health-care system and the senior citizen population.
References: